Chronic Fatigue Syndrome
Hala Abdelkarim Bakro, Muhammad Waleed Abdulrahman, Youmna Hassan Hashim, Mandy Moien Mohamed
Chronic Fatigue Syndrome
Have you ever experienced a continuous sensation of tiredness and fatigue, even after plenty of rest or sleep? It’s easy to blame yourself for laziness or procrastination, but there might be a medical reason behind it: chronic fatigue syndrome (CFS).
What is chronic fatigue syndrome:
Chronic fatigue syndrome, also known as myalgic encephalomyelitis (ME/CFS), is a long-term illness characterized by extreme exhaustion that persists even when bedridden, in addition to a significant reduction in previously tolerated activities. It can start slowly or suddenly and might continue for several years (1).
Prevalence:
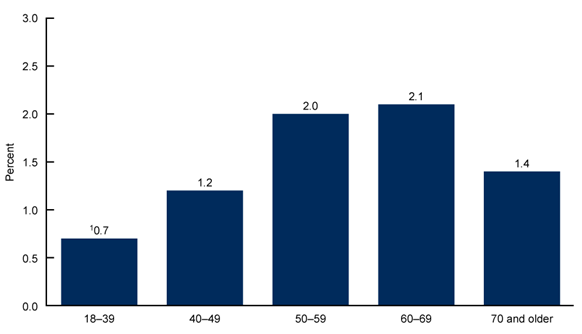
The prevalence varies according to age, gender, and race. Age-wise, CFS is more prevalent among seniors between 50 and 69 years old, while it is less prevalent among younger people (Figure 1). On the other hand, according to gender, CFS is more prevalent among women than men (2).
Diagnosis:
A CFS diagnosis is an exclusion diagnosis; it excludes other medical diseases, such as mental health issues, to confirm CFS.
To be diagnosed with CFS, the following three symptoms must have been present for over six months; additionally, the symptoms must be moderately to severely severe for at least half of the time (3).
- Fatigue: A discernible decline in a patient’s capacity to participate in activities they used to enjoy. This disability lasts longer than six months and is accompanied by sudden, intense exhaustion that doesn’t go away with rest or exercise.
- Post-exertional malaise: After being exposed to physical or cognitive stressors that they had previously accepted well, patients report worsening symptoms and function.
- Unrefreshing sleep: Following a night’s sleep, patients experience fatigue.
One of the extra symptoms listed below and the three symptoms listed above must meet the diagnosis criteria (3).
- Cognitive impairment: Issues related to thought processes or executive function exacerbated by effort, stress, or deadline pressure.
- Orthostatic intolerance: Symptoms worsen when one assumes and keeps an upright position. Placing the feet up or lying back down helps alleviate some symptoms, but they may not completely disappear.
Etiology
The starting point in the management process of any disease is to investigate the cause of the illness. The etiology of chronic fatigue syndrome is still unclear. However, according to the performed studies, they can be simplified into six main causes as follows (4):
- Genetic
A case-control study results suggested that the peripheral blood mononuclear cell gene expression is different between patients with CFS and the control group.
- Infection
In the 20th century, the first suspicion was a viral infection by the pathogen Epstein-Barr virus (EBV). However, human herpes virus-6 (HHV-6) and the human parvovirus B19 are also assumed to trigger CFS.
- Immunity
Up to date, there is no proven relation between immunological disturbances and CFS, even though some patients present with abnormal immunity in the form of reduced mitogenic response of lymphocytes and decreased complement levels.
- Endocrinology
Some researchers reported alterations of the hypothalamus-pituitary-adrenal axis, characterized by low cortisol levels in the blood fluids of patients with CFS.
- Musculoskeletal
A recent experimental study reported that patients with CFS were weaker after evaluating their performances following maximum voluntary contractions.
- Nervous System
Experiments using different imaging techniques indicated alterations in brain glucose metabolism, cortical and brain stem perfusion, and motor activities in patients with CFS.
Treatment
Pharmacological and non-pharmacological were tried to treat the most critical symptom of CFS, which is fatigue.
- Pharmacological (5):
- Antidepressants, including selective serotonin reuptake inhibitors (SSRI) such as fluoxetine and paroxetine, and Serotonin-Norepinephrine Reuptake Inhibitors (SNRI), were found to be very useful in treating depressive symptoms.
- Nervous system stimulants such as methylphenidate effectively reduced fatigue and concentration disturbances.
- Other medications, such as antivirals, corticosteroids, and immunoglobulin, were tested in different studies; however, their effects were not proven to elucidate CFS symptoms.
- Non-pharmacological (6):
- Cognitive behavioral therapy (CBT) is a type of psychotherapy that aims to manage problems by changing the behavior.
- Graded exercise therapy (GET) is a program of physical activity that gradually increases its strength and duration.
- Adaptive pacing therapy (APT) is to train the patient on balancing between rest and activity in a way that enables the patient to avoid flare-ups.
How can CFS patients cope with the disease:
Coping with CFS requires a multifaceted approach that addresses the physical and emotional challenges it presents. Here are some effective coping techniques (7-9):
- Emotion-Focused Coping: Recognize and manage emotional responses to stress caused by CFS. Practice relaxation techniques such as deep breathing exercises, meditation, or yoga.
- Problem-Focused Coping: Identify and address stressors that exacerbate CFS symptoms. Consider changing your environment, relationships, or daily routine.
- Seeking Social Support: Join support groups or online forums to share experiences, offer encouragement, and learn from others with CFS.
- Pacing and Activity Management: Balance rest and activity! CFS patients need to manage their energy levels carefully, establish boundaries, and avoid overexertion.
- Keeping Diaries: Monitor symptoms and identify activities that trigger flare-ups. This information can help you adjust your daily routine accordingly.
- Seeking Professional Assistance: Rehabilitation specialists, exercise physiologists, or therapists can provide support and guidance.
- Facilitating Activity: Explore ways to simplify daily tasks, such as using assistive devices, breaking down chores into smaller steps, or delegating responsibilities.
- Sleeping Enough: Establish good sleep habits. Create a conducive sleep environment, maintain a regular sleep-wake cycle, and avoid caffeine or alcohol before bed.
- Other Considerations: Exercise: While standard exercise recommendations may be harmful to CFS patients, it is still important to engage in activities that you can tolerate. Avoidance: Identify and avoid triggers that worsen your CFS symptoms.
Remember, coping with CFS is an ongoing process that requires patience and self-care. By implementing these techniques, individuals with CFS can manage their symptoms and improve their quality of life.
References:
- https://www.hopkinsmedicine.org/health/conditions-and-diseases/chronic-fatigue-syndrome#:~:text=It%20is%20associated%20with%20heavy,(like%20sitting%20or%20standing).
- https://www.cdc.gov/nchs/products/databriefs/db488.htm#:~:text=Key%20findings-,Data%20from%20the%20National%20Health%20Interview%20Survey,those%20age%2070%20and%20older.
- Sapra A, Bhandari P. Chronic Fatigue Syndrome. [Updated 2023 Jun 21]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK557676/
- Holgate ST, Komaroff A, Chronic Fatigue Syndrome: understanding a complex illness , Natural Reviews Neuroscience 12(9), 539-544, 2011.
- Pae CU,Marks DM, Patkar AA , Pharmacological treatment of chronic fatigue syndrome: focusing on the role of antidepressants,Expert opinion on pharmacotherapy 10(10), 1561-1570,2009.
- Wyller VB, The chronic fatigue syndrome – an update ,Acta Neurologica Scandinavian, 2007.
- https://www.nhs.uk/conditions/chronic-fatigue-syndrome-cfs/treatment/#:~:text=If%20you%20have%20mild%20or,1%2Dto%2D1%20basis.
- https://www.cdc.gov/me-cfs/living-with/index.html
- https://www.webmd.com/chronic-fatigue-syndrome/tips-living-with-chronic-fatigue